2019-05-19
 What should I eat? - One of the most common questions asked by Inflammatory Bowel Disease (IBD) patients. The role of diet has become increasingly important in the prevention and treatment of IBD.[1] In recent research, changes in the human gut microbiome have been detected in different forms of IBD such as Crohn’s disease (CD) and ulcerative colitis (UC), supporting the hypothesis of dysbiosis as a relevant component to IBD pathogenesis.[2] Researchers discovered that the gut microbiome of African children were rich in Bacteriodetes and poor in firmicutes and Enterobacteriaceae, while the results obtained from European children was the opposite due to differences in their diet.[3]
What should I eat? - One of the most common questions asked by Inflammatory Bowel Disease (IBD) patients. The role of diet has become increasingly important in the prevention and treatment of IBD.[1] In recent research, changes in the human gut microbiome have been detected in different forms of IBD such as Crohn’s disease (CD) and ulcerative colitis (UC), supporting the hypothesis of dysbiosis as a relevant component to IBD pathogenesis.[2] Researchers discovered that the gut microbiome of African children were rich in Bacteriodetes and poor in firmicutes and Enterobacteriaceae, while the results obtained from European children was the opposite due to differences in their diet.[3]
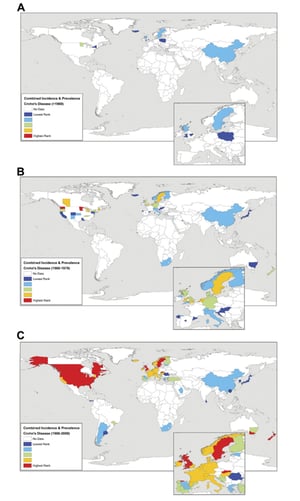
Animal fat and carbohydrate based diets lead to specific enrichment of Bacteriodes and Prevotella in adults. Typical western diets have been associated with low microbial diversity in the gut, in contrast to other diets around the world. This “western lifestyle” triggers intestinal inflammation and caused a dramatic increase in IBD in the last half-century.[2] Throughout the years, many countries have begun to adapt the western lifestyle, increasing IBD incidence (see maps highlighting world-wide increase in CD from 1960 to 2008. Study performed by Ruemmele F. M. (2016)). [3]
Exclusion diets, such as specific carbohydrate diet (SCD), paleo diet, anti-inflammatory diet, low-FODMAP diet etc., have become popular for reducing IBD. Many lay books have been published over the years claiming that some of these diets are the best solution to reduce IBD. But are they?
In today’s blog to recognize World IBD Day, we will be looking into the two most popular IBD diets: SCD and the low-FODMAP diet to determine whether they are as successful as the lay books claim them to be.
Specific carbohydrate diet (SCD)
SCD was based on a theory that disaccharides and polysaccharides pass undigested into the gut, resulting in bacterial and yeast overgrowth creating an over-production of mucus. This malabsorption was suggested to cause intestinal injury. To prevent more damage, a strict diet was recommended. SCD allows consumption of only monosaccharides (glucose, fructose and galactose) and restricts the intake of simple carbohydrates. Although, this diet is known to be quite difficult to sustain.[1]
| Food Group | Include | Avoid |
| Grains | None | All cereal grains |
| Fruit | All but canned or frozen | None |
| Vegetables | All but canned or frozen | Potato, yam, corn |
| Proteins | All others | Processed, canned or smoked meats |
| Nuts, seeds, legumes | Lentil, split pea | Most legumes (eg. Chickpeas) |
| Dairy | Lactose free | All others |
| Beverages | Wine | Milk, tea, instant coffee, soybean milk, beer |
| Other | Saccharin, honey, butter | Chocolate, margarine, corn syrup |
Table 1. Characteristics of the specific carbohydrate diet. Study done by Gottschall E, referenced by Knight-Sepulveda et al. It describes the included and excluded food groups for this particular diet.[1]
A study by Godny et al. evaluated the short-term effects of SCD with IBD patients:
- There was a rapid change in abundance of several microbial taxa, specifically a decrease in Haemophilus after one week.
- The abundance of Klebsiella/Enterobacter genus, from the Enterobacteriaceae family, increased after one week.
What is interesting is that Enterobacteriaceae is known to be associated with a high-fat diet, yet patients reported to have a greater improvement in symptoms after SCD. Therefore, the effect of SCD on inflammatory markers was considered ambiguous.[4]
Another important factor to note is that SCD is known to have the potential to cause vitamin D deficiency, which is an important concern because the human body needs sufficient vitamin D for immune function, particularly in the digestive tract.[3]
The low-FODMAP diet
The low-FODMAP diet eliminates foods that are high in FODMAPs (fermented oligo-, di-, and monosaccharide and polyol carbohydrates). Though it is a very restrictive diet, it has been reported to be successful with the majority of IBD patients. It is similar to SCD however, the difference between the two is that the low-FODMAP diet is more restrictive.[3]
| Food Group | Include | Avoid |
| Grains | Gluten-free, oat, rice, quinoa | Wheat, barley, rye |
| Fruits | Banana, blueberry, cantaloupe, clementine, grape, kiwi, lemon, lime, mandarin, melons (variety), orange, passion fruit, pineapple, raspberry, and strawberry. | Apple, apricot, blackberry, canned fruit, date, dried fruit, grapefruit, mango, nectarine, pear, peach, plum, prune, and watermelon. |
| Vegetables | Alfalfa, bean sprout, bell pepper, bok choy, broccoli (≤1/2 cup), Brussels sprout (≤ 2 sprouts), carrot, corn, cucumber, eggplant, green bean, kale, lettuce, potato, spinach, spring onion (only green top), squash, tomato, turnip, and zucchini. | Artichoke, asparagus, avocado, beetroot, cauliflower, cabbage, garlic, leek, mushroom, onion, pea, shallot, snow pea, sweet corn, sweet potato. |
| Proteins | All others | Breaded meat or meat made with HFCS. |
| Nuts, seeds, legumes | Almond (≤ 10 nuts), chia seed, nut butter, macadamia, peanut, pecan, pumpkin seed, walnut. | Bean, cashew, chickpea, lentil, pistachio, soybean. |
| Dairy | Lactose-free yogurt and milk; almond, coconut, rice, or soy milk (from soy protein); hard and low-lactose cheese. | Cow, goat, sheep, condensed, and evaporated milk; buttermilk; soy milk (from soy-bean); soft-cheese and cream. |
| Beverages | Fruit and vegetable juice made with allowed foods (limit to ½ cup at a time), wine (5 fl oz), vodka, gin (1.5 fl oz) | Coconut water, green tea, rum, soft drinks, sports drinks, white tea. |
| Other | Brown sugar, dark chocolate, maple syrup, golden syrup, stevia | Milk chocolate, sweeteners ending in “ol”, honey, HFCS. |
Table 2. Characteristics of the low-FODMAP diet. Study by Gibsen PR et al, referenced by Knight-Sepulveda et al. It describes the included and excluded food groups for this particular diet.[1]
Pedersen et al., studied the change in gut microbiota in IBD patients before and after 6 weeks of the low-FODMAP diet. Their results:
- 70% of patients were dysbiotic at baseline and 50% of patients were dysbiotic at week 6.
- Patients claimed that there was a significance improvement in their symptoms from week 0 to week 6.
They determined that the low-FODMAP diet decreases gut microbiome dysbiosis for only half of the patients and all claimed to have significantly improved symptoms, despite only 50% of patients having a reduce dysbiosis.[1]
Conclusion
These studies indicate that the impact of both the SCD and low-FODMAP diet on IBD is inconclusive. While many patients described their symptoms as improving, analysis of their gut microbiome did not reflect these improvements. Therefore the authors conclude that more studies need to be conducted.
When it comes to studying the diet and IBD, the study of the gut microbial changes is crucial to help determine whether these diets actually work. When collecting stool for these studies, it is important to have the best collection method to ensure you receive the best results. The OMNIgene·GUT self-collection kit provides the means to effectively collect and stabilize microbiome profiles from donors undergoing dysbiosis. The intuitive design of the optional spoon accessary combined with OMNIgene·GUT allows for an easier collection process and in home use for donors.[2]
“Commercially available systems [like] OMNIgene·GUT… are optimal tools for the assessment of human faecal microbiota composition and are being used in the MINUTE for IBD project due to their high convenience and reliability.” – Panek et al.[3]
For more information regarding the use of OMNIgene·GUT and IBD studies, please read our blog Collect and stabilize gut microbiota samples from IBD patients undergoing dysbiosis or contact us to request free OMNIgene·GUT collection kits for evaluation.
References
[1] Pedersen et al. Gut microbiota in IBD patients with IBS Before and After 6 weeks of low FODMAP diet. Gastro J. 146(5): S-241. (2014).
[2] https://www.dnagenotek.com/US/pdf/PD-WP-00056.pdf
[3] Panek et al. Translational research in Croatia – combining clinical knowledge and advanced technologies for studying IBD. Croatian Science Foundation. Poster. (2016).
[4] Knight-Sepulveda et al. Diet and inflammatory bowel disease. Gastroenterol Hepatol (NY). 11(8): 511-520 (2015).
[5] Rapozo DCM et al. Diet and microbiota in inflammatory bowel disease: the gut in disharmony. World J Gastroenterol. 23(12):2124-2140 (2017).
[6] Ruemmele FM. Role of diet in inflammatory bowel disease. Annals Nut Metab. 68(1). Web. (2016).
[7] Godny et al. Dietary interventions may modify intestinal inflammation via altering microbial composition – a cross over trial. Journal of Crohn's and Colitis. 12(1): S563. (2018).